You’ve probably noticed that your blood sugar doesn’t just respond to food—it responds to life. A busy morning, a tense conversation, or even a poor night’s sleep can send your glucose climbing, even when your diet hasn’t changed.
If you’ve ever watched your continuous glucose monitor (CGM) spike during a stressful moment—or felt a wave of fatigue, irritability, or hunger after a long day of “pushing through”—you’ve seen firsthand how stress biology affects your metabolism.
Let’s unpack how this works, why it matters, and how you can start breaking the stress–glucose cycle with realistic, research-backed tools.

The Stress–Glucose Connection
When your brain perceives a threat, whether it’s an overflowing inbox or a near-miss in traffic, your adrenal glands release cortisol and adrenaline. These hormones tell your liver to release stored glucose (glycogen) into the bloodstream to give you quick energy to “fight or flee.”
The problem is: in modern life, most of our “threats” are psychological or emotional—not physical. So, instead of running from danger, we stay seated at our desks while our blood sugar and stress hormones remain elevated.
Chronically elevated cortisol can make your cells less responsive to insulin, the hormone that helps glucose move into your cells for energy. This insulin resistance keeps glucose circulating in the blood longer, often leading to fatigue, brain fog, and cravings for quick energy sources—usually sugar or refined carbs .
Several studies have confirmed this relationship, showing that people with high perceived work-related stress tend to have higher fasting and post-meal glucose levels .
How Stress Impacts Your Metabolism
Over time, frequent stress responses can create a cascade of metabolic effects:
- Increased insulin resistance: Cortisol and adrenaline temporarily block insulin’s action, making it harder for your cells to absorb glucose.
- Higher blood sugar variability: Wide swings in glucose (known as glycemic variability) have been linked to oxidative stress, inflammation, and vascular dysfunction—even when average glucose remains “normal.”
- Altered hunger and satiety cues: Cortisol stimulates appetite and increases cravings for energy-dense foods, which compounds glucose fluctuations.
- Sleep disruption: Elevated evening cortisol delays melatonin release, reducing sleep quality. Poor sleep, in turn, raises cortisol again, completing a vicious cycle.
This creates what I call a metabolic feedback loop: stress raises glucose → poor glucose control leads to fatigue and anxiety → fatigue makes us more stressed. Over time, this can contribute to prediabetes, hormonal imbalances, and weight resistance.
The Cognitive and Emotional Side
It’s not just physical. Stress-driven glucose changes also affect your brain. Elevated glucose and insulin resistance in the brain can impair neurotransmitter balance, particularly serotonin and dopamine, contributing to low mood, irritability, and difficulty concentrating.
Research has even found that insulin resistance in the brain can blunt feedback to stress-regulating centers, making it harder to calm down once you’re triggered . In other words, the more metabolically stressed you become, the harder it is to emotionally self-regulate.
What the Science Says
- In a study of insulin-resistant adults, 20 minutes of daily diaphragmatic breathing lowered fasting and post-meal glucose within nine weeks .
- Another trial found that people with heart disease who practiced meditation twice per week for six months significantly improved fasting glucose, post-meal glucose, and A1c.
- Even short bouts of movement—like three 15-minute walks after meals—were more effective for blood sugar control than one longer session per day .
- And after just five nights of sleep restriction, healthy young men showed metabolic profiles resembling early-stage diabetes, with slower glucose clearance and increased insulin resistance .
These findings show how deeply connected our nervous system and metabolism really are.
Practical Steps to Break the Cycle
1. Reframe stress as a signal—not an identity
You can’t eliminate stress, but you can retrain your response. When stress hits, your goal is to activate your parasympathetic nervous system (“rest and digest”) instead of staying in fight-or-flight.
Try this: Sit tall, place one hand on your belly, inhale through your nose for a count of 4, and exhale slowly for 6–8 counts. Repeat for 3–5 minutes. This simple practice lowers cortisol and glucose while calming your mind.
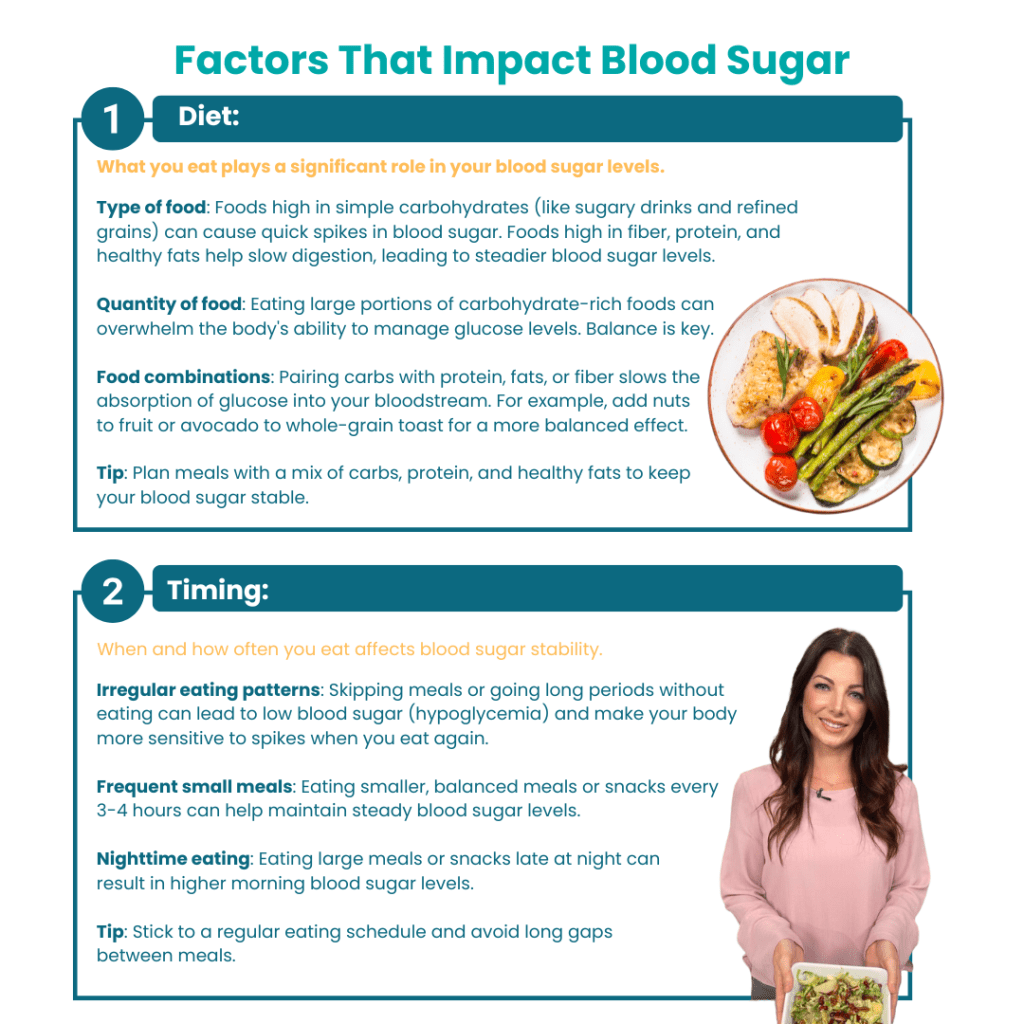
2. Build “glucose-buffering” meals
Start your meals with vegetables or protein to slow digestion and reduce post-meal spikes. Pair complex carbs with fiber, protein, or healthy fats to keep blood sugar—and mood—steady.
Example:
- Instead of toast and jam → try avocado toast with an egg.
- Instead of a smoothie of just fruit → add Greek yogurt, chia seeds, and leafy greens.
Aim for roughly 30% of calories from protein, 35% carbs (mostly from whole foods), and 35% fat, with at least 25–30g of fiber daily.
3. Move when it matters
You don’t need long workouts to improve metabolic control. Even low-intensity movement, such as walking after meals or gentle yoga in the evening, can blunt glucose spikes and lower cortisol.
Tip: Try 10–15 minutes of walking within 30–60 minutes after eating—it helps muscles use glucose and supports digestion.
4. Prioritize restorative sleep
Consistent, high-quality sleep is one of the most powerful metabolic regulators. Aim for 7–8 hours per night. Protect your sleep environment: cool, dark, and device-free for at least 60 minutes before bed.
If you’re waking wired or anxious, consider magnesium glycinate or relaxation rituals (breathing, stretching, herbal tea) to support cortisol balance.
5. Support your “quiet” levers
Micronutrients like magnesium, selenium, and vitamin B6 play critical roles in insulin signaling and stress resilience .
Likewise, supporting gut health with prebiotic fibers, probiotics, and a diverse plant-based diet helps regulate inflammation and improve glucose control.
Even environmental factors—like exposure to endocrine-disrupting chemicals (e.g., BPA)—can worsen insulin resistance , so choose glass or stainless-steel containers when possible and minimize processed foods.
Connecting the Dots: Data and Awareness
If you wear a CGM, notice the patterns:
- Do your glucose spikes correlate with emotional stress or work intensity?
- How does your post-meal walk or breathing exercise affect recovery time?
- Do sleep-deprived days look different from well-rested ones?
These insights can help you understand your body’s unique stress–metabolism relationship—and guide you to personalized interventions that actually stick.
Final Thoughts
Stress may be inevitable, but metabolic chaos doesn’t have to be.
By tuning into your body’s responses and building simple, consistent habits—structured meals, mindful breathing, restorative sleep, and gentle movement—you can train your nervous system to stay calm and your blood sugar to stay stable.
Small steps practiced daily build resilience that lasts.
If you’d like help identifying patterns or personalizing a nutrition and stress-resilience plan based on your labs or CGM data, I can help you translate that information into action—so your body works with you, not against you.
References
- Levels Health. How Does Stress Affect My Glucose Levels? Updated Oct 14, 2024.
- Levels Health. The 7 Factors That Significantly Impact Your Blood Sugar. Updated Sept 11, 2023.
- DiPietro L. et al. Three 15-min bouts of moderate post-meal walking vs one 45-min walk: 24-h glycemic control.Diabetes Care, 2013.
- Buxton OM et al. Sleep restriction for one week reduces insulin sensitivity in healthy men. Diabetes, 2010.
- Obaya HE et al. Effect of aerobic exercise, slow deep breathing, and mindfulness meditation on glucose and cortisol in T2D. 2023.